Healthcare workers operate in environments where the risk of exposure to bloodborne pathogens is a significant concern. Bloodborne pathogens (BBPs) are infectious microorganisms in human blood that can cause disease in humans. The primary pathogens of concern include hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV). This article delves into the most common risk of exposure to these pathogens for healthcare workers, examines the associated risks, and discusses strategies for prevention and management.
Types of Bloodborne Pathogens
- Hepatitis B Virus (HBV): HBV is a major cause of liver infection and is highly infectious. It can be transmitted through exposure to infectious blood or other body fluids. The virus can lead to chronic liver disease and increases the risk of liver cancer.
- Hepatitis C Virus (HCV): HCV primarily affects the liver and can lead to chronic liver disease. Unlike HBV, HCV does not have a vaccine, making prevention particularly critical.
- Human Immunodeficiency Virus (HIV): HIV attacks the immune system, specifically the CD4 cells, which can lead to acquired immunodeficiency syndrome (AIDS). While there is no cure for HIV, antiretroviral therapy can manage the infection effectively.
Common Risks of Exposure
Healthcare workers are at risk of exposure to bloodborne pathogens through various mechanisms. Understanding these risks is crucial for implementing effective prevention measures. Here are some of the most common risks:
-
Needle Stick Injuries
Needle stick injuries are one of the most common risks of exposure to bloodborne pathogens. These injuries occur when a needle or other sharp instrument accidentally punctures the skin, potentially transferring infectious blood from a patient to the healthcare worker. According to the Centers for Disease Control and Prevention (CDC), needle stick injuries are responsible for the majority of occupational exposures to BBPs in healthcare settings.
Prevention Strategies:
- Use of Safety-Engineered Devices: These devices are designed to minimize the risk of injury. Examples include needleless systems and safety syringes.
- Proper Disposal: Ensuring that sharps are disposed of in appropriate, puncture-resistant containers immediately after use.
- Training and Awareness: Regular training programs on safe needle practices and the proper handling of sharps.
-
Blood Spills and Contaminated Surfaces
Blood spills and contaminated surfaces pose a risk of exposure if they come into contact with broken skin or mucous membranes. For instance, cleaning up blood spills without appropriate protective equipment or not properly disinfecting surfaces can lead to infections.
Prevention Strategies:
- Use of Personal Protective Equipment (PPE): Gloves, gowns, and face shields should be worn when dealing with blood spills or contaminated surfaces.
- Effective Disinfection Protocols: Regular and thorough cleaning of surfaces and equipment with appropriate disinfectants.
-
Exposure through Open Wounds or Broken Skin
Healthcare workers with open wounds or broken skin are at higher risk of infection if they come into contact with bloodborne pathogens. This can occur during procedures, when handling contaminated materials, or through accidental contact with blood.
Prevention Strategies:
- Proper Wound Care: Ensuring that any cuts or abrasions are covered with waterproof bandages.
- Hand Hygiene: Frequent and thorough hand washing, especially before and after patient contact.
-
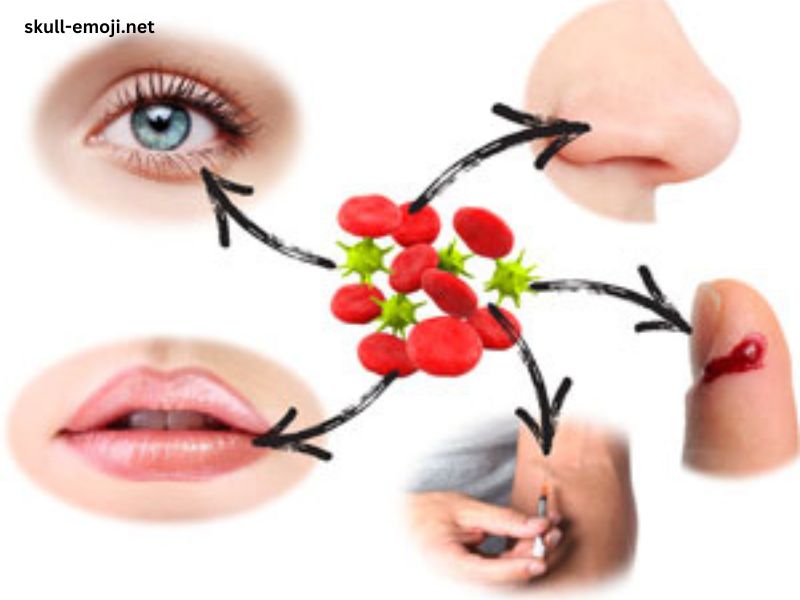
Mucous Membrane Exposure
Exposure to bloodborne pathogens can also occur if blood or other potentially infectious materials come into contact with mucous membranes such as the eyes, nose, or mouth. This risk is often associated with procedures that involve splashing or spraying of blood.
Prevention Strategies:
- Use of Protective Barriers: Face shields or goggles should be worn during procedures with a high risk of splashing.
- Immediate Rinsing: If exposure to mucous membranes occurs, the affected area should be rinsed with water or saline immediately.
-
Inadequate Training and Knowledge
Inadequate training and knowledge about BBP risks and prevention measures can lead to higher rates of exposure. Healthcare workers who are not well-versed in proper procedures are more likely to experience accidents and exposure incidents.
Prevention Strategies:
- Regular Training Programs: Conducting comprehensive training sessions on BBP risks, preventive measures, and the correct use of PPE.
- Update Policies and Procedures: Keeping up-to-date with the latest guidelines and standards for preventing exposure.
Legal and Regulatory Framework
Healthcare facilities are required to comply with regulations designed to protect workers from exposure to bloodborne pathogens. In the United States, the Occupational Safety and Health Administration (OSHA) has established the Bloodborne Pathogens Standard, which outlines requirements for minimizing exposure risks. Key components of this standard include:
- Exposure Control Plan: Facilities must have a written plan that outlines procedures for minimizing exposure risks, including the use of PPE and safe handling practices.
- Vaccination Requirements: Facilities are required to offer hepatitis B vaccinations to employees who have a potential for occupational exposure.
- Post-Exposure Evaluation and Follow-Up: There must be protocols in place for evaluating and providing follow-up care after an exposure incident, including testing and counseling.
Management of Exposure Incidents
When an exposure incident occurs, immediate action is essential to mitigate the risk of infection. The following steps should be taken:
- Immediate Cleaning: The affected area should be washed thoroughly with soap and water, and any contaminated surfaces should be cleaned according to protocols.
- Report the Incident: The exposure should be reported to the appropriate personnel within the healthcare facility as soon as possible.
- Medical Evaluation: The exposed worker should seek medical evaluation to assess the risk of infection and receive appropriate treatment, which may include post-exposure prophylaxis (PEP) for HIV.
- Documentation: Detailed documentation of the incident should be maintained, including the circumstances of the exposure and the actions taken.
- Follow-Up Testing: Regular follow-up testing for BBPs may be required to monitor for potential infections.
Conclusion
The most common risk of exposure to bloodborne pathogens for healthcare workers primarily involves needle stick injuries, blood spills, contaminated surfaces, and contact with mucous membranes. Understanding these risks and implementing effective prevention strategies are crucial for safeguarding the health and safety of healthcare workers. Compliance with regulatory requirements, ongoing training, and prompt management of exposure incidents are essential components of a comprehensive approach to preventing and managing bloodborne pathogen exposure. By prioritizing these measures, healthcare facilities can significantly reduce the risk of infection and protect their workforce from the potentially serious consequences of bloodborne pathogens.